Calming the Storm: Understanding and Reducing Stress in ME/CFS, Long Covid, and Fibromyalgia
- Sue Wharton
- Dec 1, 2025
- 8 min read
Living with a long-term illness such as Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS), Long Covid, or Fibromyalgia often means living with a body and mind under constant pressure. Stress becomes not just an emotional response, but a physical burden that interacts with every system in the body — amplifying symptoms, draining energy, and challenging recovery.
This article explores why stress is such a major factor in these conditions, how it shows up, and the most effective ways to calm the body’s overactive stress response. We’ll look at what the research says about relaxation and mind-body strategies — and how to adapt them safely for those with energy-limiting conditions.

Understanding Stress in ME/CFS, Long Covid, and Fibromyalgia
Everyone experiences stress, but for people with chronic fatigue–related conditions, it can feel like the stress system itself is stuck in overdrive.
The biology of chronic stress
When we face a challenge or threat, our nervous system activates the fight-or-flight response: adrenaline surges, heart rate increases, and muscles tense in preparation for action. Normally, this system switches off when the threat passes.
In ME/CFS, Long Covid, and Fibromyalgia, research suggests that the stress-response system (the HPA axis and autonomic nervous system) may become dysregulated (1). Studies have found:
Blunted cortisol responses — people with ME/CFS often produce lower levels of cortisol throughout the day, a pattern linked with chronic fatigue and poor stress recovery.
Autonomic imbalance — reduced parasympathetic (“rest and digest”) activity and increased sympathetic (“fight or flight”) tone.
Heightened pain and fatigue sensitivity — the nervous system becomes more reactive, amplifying pain, fatigue, and sensory overload.
This means that what might be a small stressor for someone else — a short conversation, a change in temperature, a noisy room — can provoke a cascade of symptoms in someone with these conditions.

Tired But Wired
Both ME/CFS and LC are characterised by low cortisol and sustained noradrenaline release. Cortisol normally helps the body turn off the stress response after activation but when cortisol levels are low, this “off switch” fails — leaving adrenaline elevated even in rest.
• Result: the body is biochemically exhausted yet hypervigilant
What ‘tired but wired’ feels like:
• A profound physical and cognitive fatigue - but inability to relax or sleep
• Racing thoughts - or a “buzzing” sensation even when lying still
• Heightened sensitivity - to light, sound, and touch
• A feeling of being “on edge” or overstimulated — as if adrenaline is still running despite exhaustion.
Although the body’s energy systems are drained, the stress response remains activated — creating a paradoxical mix of collapse and alertness.
The Many Faces of Stress
1. Physical Stress
Energy limitation is the defining feature of ME/CFS and often present in Long Covid and Fibromyalgia. Even small exertions — walking across a room, concentrating on an email, or doing light chores — can push the body into a state of post-exertional malaise (PEM).
This physical stressor can cause:
Deep muscle pain and heaviness
Worsening fatigue after activity
Sleep disturbance
Dizziness or heart palpitations (often related to dysautonomia or POTS)
2. Cognitive Stress
Cognitive dysfunction (“brain fog”) can make everyday tasks — reading, decision-making, or conversation — feel overwhelming. The frustration of losing mental clarity often adds emotional stress, feeding a sense of anxiety or helplessness.
3. Emotional Stress
Chronic illness brings profound uncertainty: fears about work, finances, relationships, and identity. The loss of independence and misunderstanding from others often lead to isolation and sadness. These emotional burdens activate the same stress pathways that influence physical symptoms.
4. Sensory and Environmental Stress
Many people with ME/CFS or Fibromyalgia experience sensory hypersensitivity — bright lights, loud sounds, or strong smells can trigger discomfort and fatigue. For those with Long Covid, overstimulation often leads to cognitive crashes and exhaustion.

How Stress Manifests in These Conditions
The line between “stress symptoms” and “illness symptoms” is blurred, because the body systems involved — the immune, endocrine, and nervous systems — are interconnected. Common manifestations include:
Increased pain and muscle tension
Flare-ups of fatigue or PEM after emotional or physical stress
Heart palpitations, dizziness, or shortness of breath (autonomic symptoms)
Sleep disruption — difficulty falling or staying asleep, or non-restorative sleep
Irritability, anxiety, or low mood
Digestive changes — IBS-like symptoms due to gut–brain axis sensitivity
Cognitive fog and reduced concentration
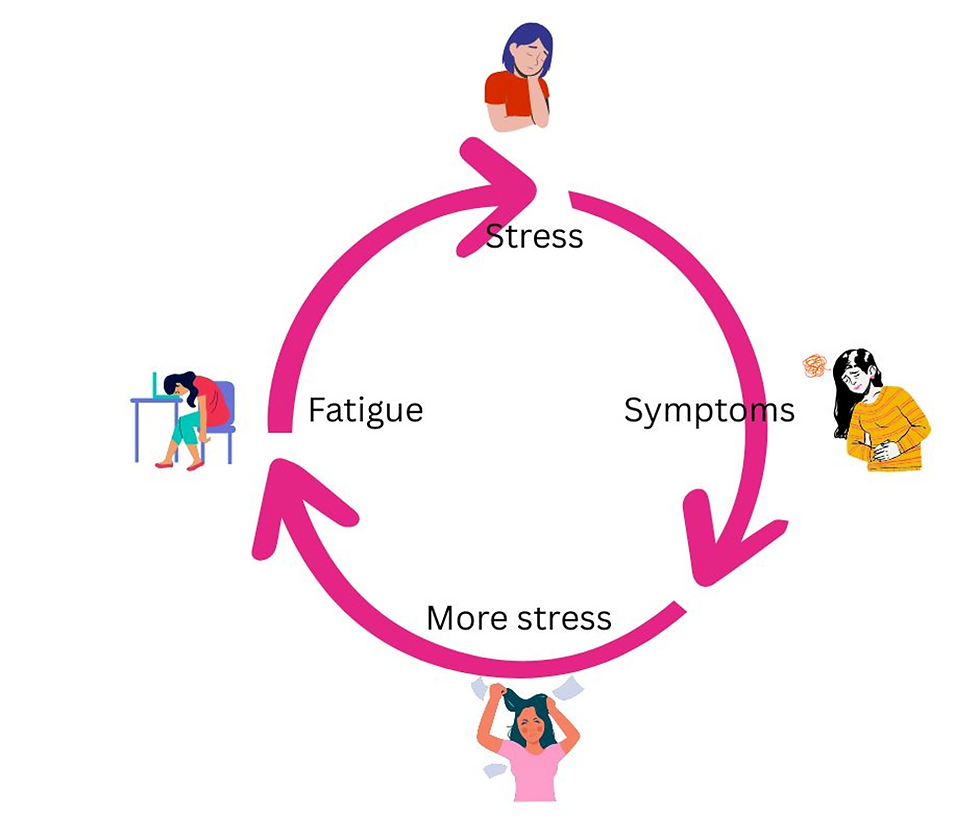
Over time, these stress reactions can create a vicious cycle: stress worsens symptoms, symptoms increase stress, and recovery becomes harder. Breaking that cycle is one of the most important aspects of symptom management.
Breaking the Stress Cycle
Your goal: interrupt the cycle through calming, pacing, and self-care activities. We can’t eliminate stress, but we can change how our bodies respond.
What the Research Says: Evidence-Based Approaches to Relaxation
Several studies have explored non-pharmacological interventions for managing stress and fatigue in these conditions. Here are key findings:
Mindfulness-based programs — A pilot randomized trial by Rimes & Wingrove (2013) found that a tailored Mindfulness-Based Cognitive Therapy (MBCT) course reduced fatigue and distress in people with CFS who had not fully recovered after CBT. Participants showed improved mood, self-compassion, and coping.(2)
Mind-body interventions — A 2021 systematic review (Ardestani et al., Medicina) reported that mindfulness, yoga, tai chi, and relaxation training produced small-to-moderate improvements in fatigue, anxiety, and quality of life for ME/CFS (3)
Guided breathing — A 2024 Scientific Reports trial found that guided breathing exercises significantly reduced anxiety and stress in COVID-19 patients. Although participants were in the acute stage of illness, the findings support the power of gentle breath regulation to calm the nervous system. (4) (5)
Heart rate variability (HRV) biofeedback — A 2024 study in the Journal of Clinical Medicine showed that HRV biofeedback improved fatigue and perceived energy in people with fibromyalgia, suggesting that retraining the balance between sympathetic and parasympathetic activity may reduce stress-related symptoms. (6)
Nature-Based Guided Imagery (GI) — A 2018 study in Frontiers in Psychology showed that nature-based GI produced significantly greater anxiety reduction than non-nature GI, suggesting that nature-based GI is an effective, cost-efficient, and accessible anxiety management intervention (7)
Sleep for stress recovery — A 2025 review in the journal Neuron, discusses how improving sleep (e.g., via sleep hygiene, CBT for insomnia) might be a promising strategy to boost stress resilience and mental‑health recovery (8)
Together, this research suggests that gentle, restorative mind-body interventions — especially those that regulate breathing, attention, and nervous system balance — can help reduce the physiological and emotional impact of stress.
Strategies for Rest and Relaxation
1. Pacing: The Foundation of Recovery
Pacing is not just about doing less; it’s about doing things strategically. It means balancing activity and rest to avoid post-exertional crashes.
Break tasks into small chunks with planned rest periods.
Use energy envelopes — stop before symptoms worsen.
Alternate physical, cognitive, and emotional tasks throughout the day.
Pacing reduces the body’s sense of “emergency” and allows the nervous system to settle into a calmer baseline.
2. Breathwork and Nervous System Regulation
Gentle breathing exercises are among the safest and most effective ways to engage the parasympathetic nervous system. Try:
Diaphragmatic breathing: Breathe slowly into your belly (in for 4, out for 6).
Resonance breathing: Aim for ~6 breaths per minute.
Guided audio or HRV biofeedback apps: These can help monitor and train your breathing rhythm.
Avoid long breath-holds or fast breathing, which can provoke dizziness or fatigue.
3. Mindfulness and Compassion Practices
Mindfulness isn’t about forcing relaxation; it’s about noticing without judgment. For people with chronic illness, mindfulness can:
Reduce catastrophizing and fear of symptoms.
Increase tolerance for uncertainty.
Enhance self-kindness and reduce perfectionism.
Short, adapted practices work best: 5–10 minutes of mindful breathing or body scanning while lying down, or brief awareness pauses during the day.
4. Progressive Muscle Relaxation and Gentle Movement
When pain or muscle tension increases, gentle movement or relaxation can help recalibrate body awareness.
Try slow stretching, restorative yoga (with full support), or guided progressive relaxation.
If physical activity triggers PEM, focus on imagery-based relaxation — mentally scanning and releasing tension without moving.
5. Sensory Grounding
Because many people with these illnesses are hypersensitive, grounding techniques can reduce sensory overload:
Lower lights and reduce noise.
Use soft textures, weighted blankets, or gentle aromatherapy (if tolerated).
Focus attention on one neutral sensory input — the feeling of your hands resting, or the
rhythm of your breath.

6. Sleep Hygiene and Restorative Rest
Stress worsens sleep; poor sleep increases stress — so focusing on restorative rest is crucial.
Keep consistent bedtime and wake-up times.
Avoid stimulating media before bed.
If you can’t sleep, practice a body scan or guided relaxation instead of forcing sleep.
Use brief “non-sleep rests” during the day — eyes closed, slow breathing, minimal stimulation.
7. Connection and Emotional Support
Chronic illness often isolates people. Emotional connection can lower cortisol and improve resilience.
Online or in-person support groups can offer understanding and validation.
Gentle talk therapy or acceptance-based approaches can help process grief and frustration.
Compassion-focused therapy or mindful self-compassion programs can build inner resilience.
Putting It All Together
Stress reduction in ME/CFS, Long Covid, and Fibromyalgia is not about “relaxing harder.” It’s about retraining an overactive system to feel safe again. The key themes are:
Gentleness: Avoid pushing the body; safety and comfort come first.
Consistency over intensity: Small, regular practices build stability.
Self-compassion: Acknowledge limitations without blame.
Integration: Rest, pacing, emotional support, and mind-body practices complement medical and physical management.
When to Seek Professional Guidance
If stress, anxiety, or trauma feel overwhelming, or if relaxation exercises trigger distress or symptom flares, it’s wise to work with a health professional familiar with energy-limiting conditions — ideally a psychologist, occupational therapist, or physiotherapist experienced in ME/CFS or Long Covid care.
They can help you adapt techniques safely, monitor responses, and develop a personalized plan that respects your energy limits.
Final Thoughts
For people with ME/CFS, Long Covid, or Fibromyalgia, stress is more than an emotional experience — it’s a biological amplifier that interacts with fatigue, pain, and cognitive function. The good news is that by understanding the body’s stress mechanisms, we can learn ways to quiet them.
Through mindful pacing, gentle breathing, compassion-based awareness, and structured rest, it’s possible to reduce the body’s sense of alarm and cultivate a quieter, steadier baseline. The path to healing is rarely linear, but every small act of calm — every moment of rest — helps the nervous system remember that safety is still possible.
Books recommended by our members:
Based on an 8-week Mindfulness-based Cognitive Therapy programme, this guide addresses the increasing need for adapted mindfulness in the management of ME/CFS, fibromyalgia, Long Covid, and other chronic fatigue conditions.
What happens when our minds and bodies are pushed beyond their limits? Vincent Deary is a health psychologist who has spent years helping his patients cope with whatever life has thrown at them. In How We Break, he has written a book for all of us who sometimes feel we have reached our breaking point.
Physiotherapist and neurophysiology expert, Jessica Maguire wants to help you understand the root cause of many of our health issues – our dysregulated nervous system. In The Nervous System Reset, Maguire explains why your vagus nerve is key to emotional, digestive and physical health, and how to engage it to help reset your nervous system.
Wintering is a poignant and comforting meditation on the fallow periods of life, times when we must retreat to care for and repair ourselves. Katherine May thoughtfully shows us how to come through these times with the wisdom of knowing that, like the seasons, our winters and summers are the ebb and flow of life.









Comments